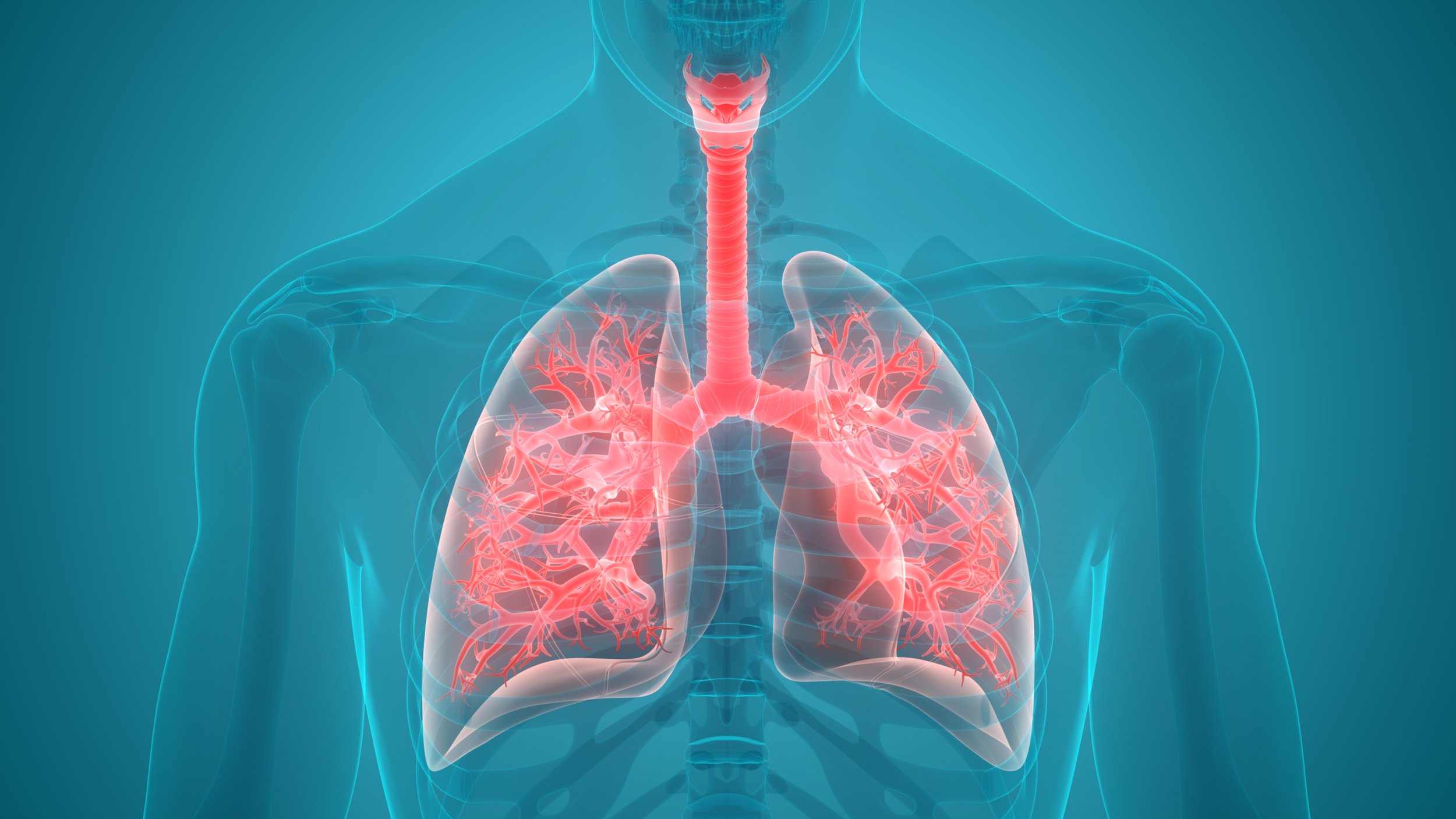
Bronchiectasis
Virtue’s services for Bronchiectasis are launching in December 2024. Pre-register your interest here.
Bronchiectasis is a long-term condition where the airways of the lungs become widened, leading to a build-up of excess mucus that can make the lungs more vulnerable to infection.
Symptons
The severity of symptoms can vary widely. Some people have only a few symptoms that do not appear often, while others have wide-ranging daily symptoms. The symptoms tend to get worse if you develop an infection in your lungs.
The most common symptom of bronchiectasis is a persistent cough that brings up a large amount of phlegm on a daily basis. The phlegm can be clear, pale yellow or yellow-greenish in colour. Some people may only occasionally cough up small amounts of phlegm, or none at all.
Other symptoms may include:
coughing up blood
shortness of breath
chest pain
wheezing noises when breathing
joint pain
clubbing of the fingertips
Signs of a lung infection
If you develop a lung infection, your symptoms usually get worse within a few days. This is known as an infective exacerbation.
It can cause:
coughing up blood
coughing up even more phlegm
chest pain
shortness of breath
feel very tired
feel generally unwell
When to seek medical advice
If you have not previously been diagnosed with bronchiectasis and you develop a persistent cough, we recommend booking an initial consultation with one of our Consultant Specialists.
While persistent coughing may not necessarily be the result of bronchiectasis, it needs further investigation.
If you have been diagnosed with bronchiectasis previously and begin to experience symptoms that suggest you have a lung infection, contact Virtue.
You'll usually need treatment with antibiotics, which we can deliver in the home.
Some people with bronchiectasis are given a stock of antibiotics as a precaution in case they suddenly develop a lung infection.
When to seek urgent medical advice
Some people with bronchiectasis develop a severe lung infection that may need to be treated by acute hospital services. Virtue offer an alternative to hospitalisation, by providing equivalent Consultant-led treatment in the home, including administering of Intravenous Antibiotics.
Signs and symptoms of a serious lung infection include:
a blueish tinge to the skin or lips (cyanosis)
confusion
a high temperature
rapid breathing (more than 25 breaths a minute)
severe chest pain that makes it too painful to cough and clear your lungs
If you experience any of the above, contact Virtue immediately to arrange an urgent consultation with a Consultant and to discuss admission to our Acute Virtual Ward.
Treatment for pneumonia
You'll usually be given antibiotics to treat pneumonia. Most people get better in 2 to 4 weeks. Some people are more at risk of becoming seriously ill. You may need to go to hospital, or be admitted to our Acute Virtual Ward for treatment if:
you're over 65
you have cardiovascular disease or a long-term lung condition
you're very unwell
In hospital, or our Virtual Ward, you'll usually be given fluids and antibiotics to treat the infection. You may also be given oxygen to help you breathe. You may be sent for an X-ray and blood tests to check for other conditions.
Things you can do if you have pneumonia
Rest until you feel better – try to stay at home and avoid contact with other people if you have a high temperature or do not feel well enough to do normal activities
drink plenty of fluids
take paracetamol or ibuprofen to help with pain or a high temperature
cover your mouth and nose with a tissue when you cough or sneeze
put used tissues in the bin as quickly as possible
wash your hands regularly with water and soap
Do not take cough medicine – coughing helps your body get rid of the infection
do not smoke

Causes of pneumonia
Pneumonia is usually caused by a bacterial or viral infection.
You can catch pneumonia from someone who has it, or you can sometimes get it if you have another infection such as:
Respiratory syncytial virus (RSV)
Flu
Covid-19
Pneumonia can be caused by a fungal infection, but this is rare in healthy people in the UK. It may also be caused by something getting into your lungs, such as water or food (aspiration pneumonia).
How to reduce your risk of pneumonia
Our Elective Remote Monitoring services can detect early signs of Pneumonia, enabling early intervention and treatment. In a lot of cases, this early intervention can avoid the onset of pneumonia, or reduce its severity considerably. If Pneumonia does develop the extent such that acute hospital treatment is required, Virtue can also provide this treatment from the comfort of home, in our Acute Virtual Ward.
There are several vaccines available to help protect you or your child from infections that can cause pneumonia:
-
recommended for babies, adults over 65 and people at higher risk of pneumococcal infections
-
recommended during pregnancy, for adults over 65, people with certain long-term health conditions and those at high risk of catching or passing on flu
Just over a quarter (28%) of people who attend a major A&E department end up being admitted into a hospital bed. In recent years, long waits for admission have reached record levels. The number of people waiting more than 12 hours after a decision to admit (sometimes referred to as ‘trolley waits’ or ‘corridor waits’) has increased from less than 150 in the first quarter of 2014 to nearly 150,000 in the first quarter of 2024. In January 2024 the average waiting time for an admission, following a decision to admit, was 6 hours and 12 minutes (source: Nuffield Trust, ‘A&E waiting times’ June 2024).
42% Percentage of A&E attendances that fail the NHS 4-hour target
6 hours 12 minutes is the average waiting time* for a hospital bed following decision to admit
-
recommended for adults aged 75 to 79, and during pregnancy (from 28 weeks onwards) to help protect your baby after they're born
-
a seasonal vaccine that's recommended for people at increased risk from COVID-19